Increase in oral dysplasia and oral cancer rates due to COVID-19 alcohol-related consumption
The COVID-19 pandemic has profoundly affected all aspects of life, including health. One of the more concerning developments is the increase in oral cancer rates because of greater alcohol consumption during this period. Research indicates that, due to financial insecurity, depression, general anxiety, and boredom surrounding the pandemic, people turned to risky behavior, most notably alcohol use, in order to cope with their increase in stress.1
Alcohol use during the COVID-19 pandemic
One study showed that although smoking rates dropped 1.1% from 15.3% to 14.2% among those aged 18-54, rates increased slightly in individuals over the age of 55.2 Alcohol use, on the other hand, increased dramatically in all age groups. In 2020, the first year of the pandemic, sales of alcohol increased by 2.9%, the largest annual increase in more than 50 years.3
Another study found alcohol-related deaths increased by 2.2% in the past 20 years prior to the pandemic, and then suddenly jumped 25.5% between 2019 and 2020, totaling 99,107 deaths.4 This same study showed alcohol-synthetic opioid-related deaths jumped a staggering 59.2% among people aged 25-44 during the pandemic.
In addition to deaths, pandemic-related increases in alcohol consumption have been associated with other negative health outcomes, such as increases in transplants for alcohol-associated liver disease,5 emergency department visits for alcohol withdrawal and excess consumption,6 as well as an increase in oral dysplasia and oral cancer diagnosis.
Alcohol use and oral cancer
The link between oral cancer and alcohol consumption is well-documented in the literature. Studies have shown that moderate alcohol consumption (two to four drinks per day) can increase the risk of oral cancer by 1.4 times that of a nondrinker. Heavy alcohol consumption (more than five drinks per day or 15 drinks per week) can increase the risk of oral cancer by 5 times that of a nondrinker.7 This risk is further exacerbated when alcohol is combined with tobacco use and smoking.8
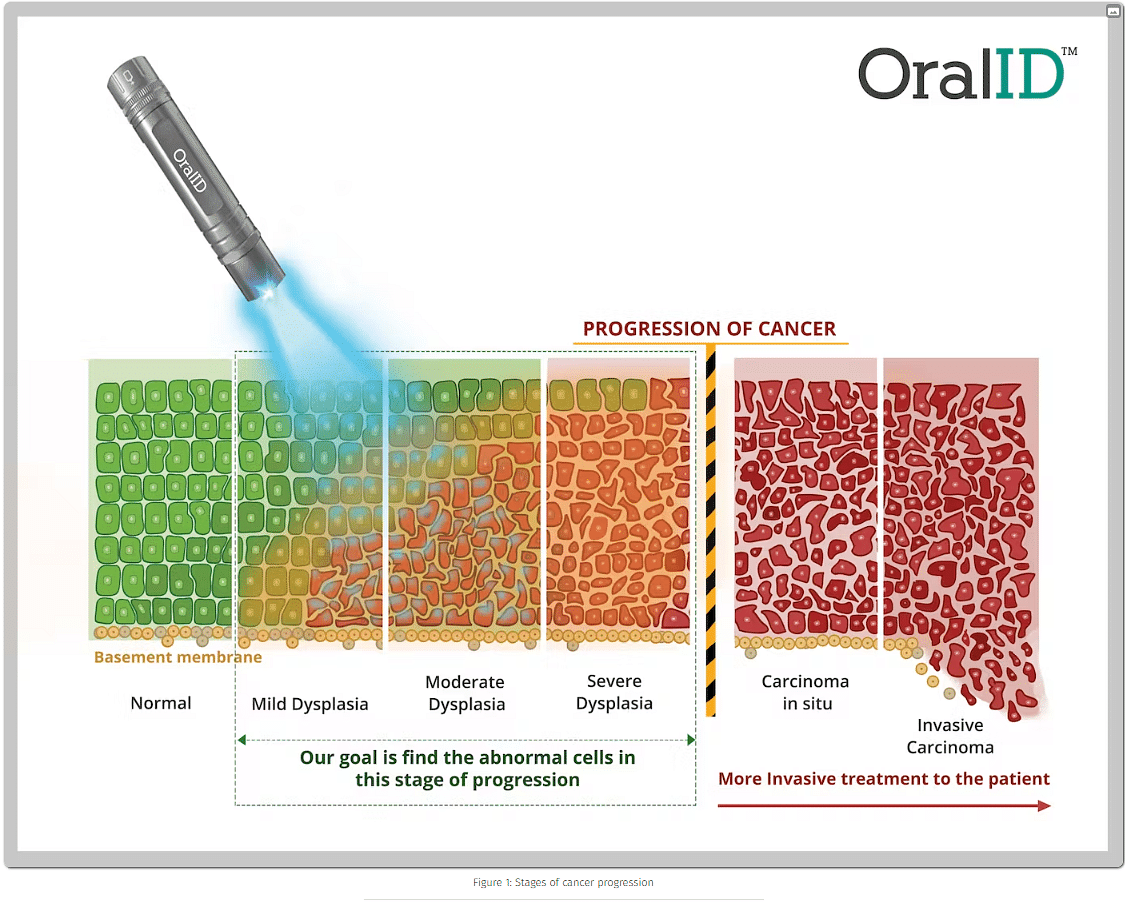
OralID and biopsy to diagnose oral dysplasia
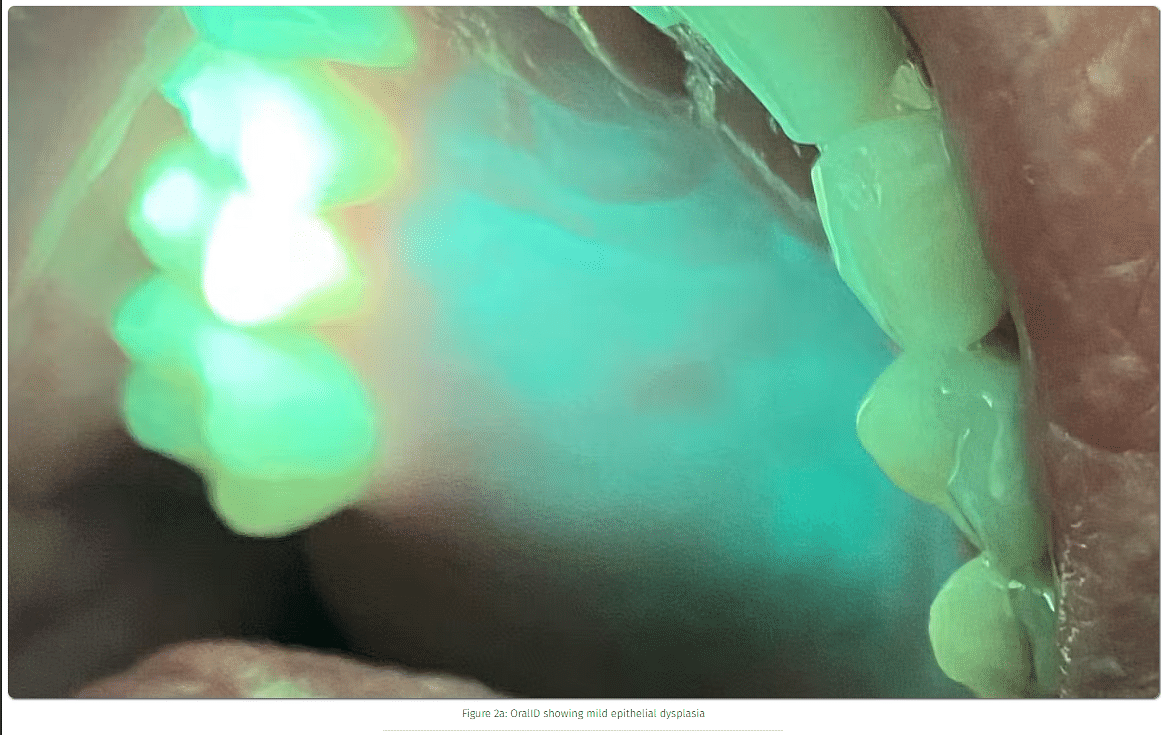
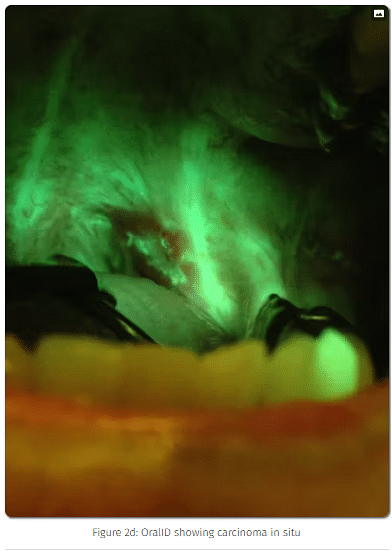
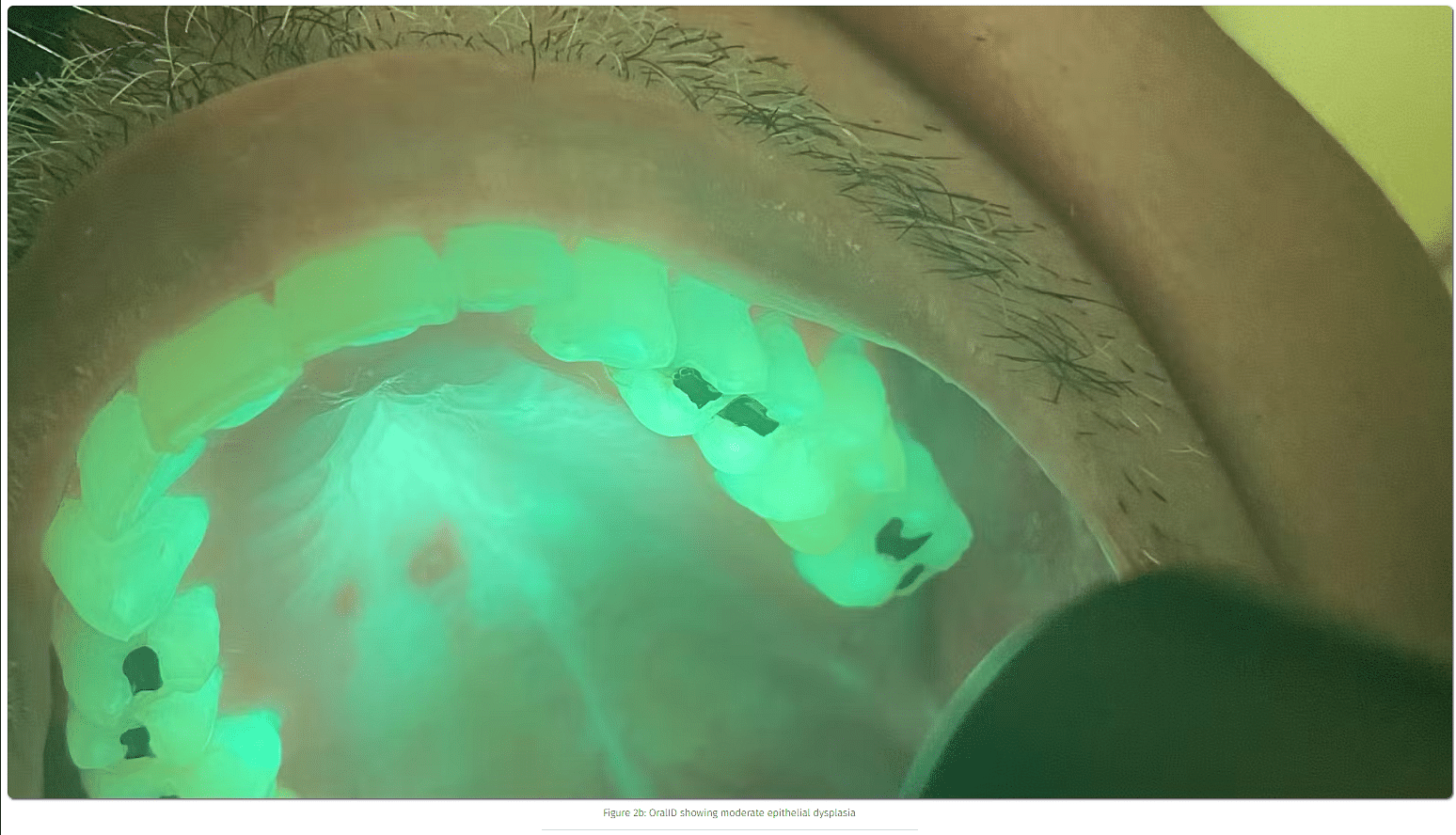
In this study, the author and colleagues identified 53 suspicious lesions (figure 1) in the oral cavity through the use of handheld autofluorescence technology (OralID). The lesions were then sent for biopsy during the period of 2021-2023. The lesions were histochemically stained and sectioned, and graded according to dysplastic progression (figures 2a-2d). Sixty-four percent of the specimens biopsied returned with a grade of mild to moderate epithelial dysplasia or higher.
About the Author
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a Naturopath Doctor with a focus on digestive health. Contact him through his website at drscottfroum.com (www.drscottfroum.com) or (212) 751-8530